How I Was Kicked Out of the ICU Advocating for my Mom with ALS
Outside my incapacitated, non-verbal, quadriplegic mothers room in the ICU — I cut off the doctor while he was berating me from feet away and told him his aggressive behavior violated my mother’s patient rights and my rights as her legal guardian.
He denied what I said, and I told him I would pull up the law right then.
As I pulled up a browser I told him he was welcome to, and he immediately raised his voice directing another staff to call security.
A guard who had already been around the corner stepped into sight and slowly walked toward my mom’s room.
This happened just a month ago on July 1st, 2025. Before I move forward I need to circle back to the end of June, because everything that happened after the guard walked toward my moms room came full circle.
I’ve submitted my formal reports. This you are reading now is my public one to bring awareness and fair warning to the potential dangers behind the closed doors of an ICU and the lengths of which this Illinois hospital went to downplay their actions. For context, my mom is 75 years old and has had advanced ALS.
For four and a half years I have lived every day with her, alongside my dad and younger sister who is high functioning on the Autism Spectrum. We are and have been her full-time caregivers and she is the center of our world.
The day I heard her diagnosis, my heart shattered. I remembered back to when I was younger. Stephen Hawking came up in conversation and mom said he had Lou Gehrig’s disease as ALS is also commonly known and explained what it was and how terrible as the disease is.
ALS is a rare neurodegenerative disease affecting about 0.0005–0.1% of the U.S. population and about 0.002%-0.006% globally.
There is currently no cure for ALS. Despite underfunding, researchers worldwide work toward finding a cure and developing medications to slow disease progression.
As the disease has progressed, I’ve watched my mom become paralyzed with only a small bit of mobility left to tilt her head slightly to the side. I’ve lived through her losing the ability to speak verbally. Learned how to program a Tobii Dynavox eye gaze tracking AAC computer software so she can talk with a synthesized voice. Learned how to crush up her pills and give her fluids through a feeding tube in her stomach. Rock her back and forth on a bedside commode (which she is no longer able to do as of the end of June after going to the hospital) and even how to suction the back of her throat when her lungs muscles deteriorated to the point she became dependent on us to make sure she didn’t drown in the mucus she couldn’t cough up by herself anymore.
More critical background information:
- Mom had been struggling with long coughing fits that required suctioning and despite mucus medication, increased nebulizer treatments and increased use of our cough assist machine. Things didn’t settle down until her home healthcare doctors took us seriously and ran an x-ray that showed clouding in her right lung.
- They prescribed one week of antibiotics which cleared the coughing fits up, and shortly after, they returned.
- The doctors ran another x-ray and they determined it was clear, no more clouding.
- Mom started to want to use her BiPAP more frequently to help her breathe easier.
- Then, she started to develop a pressure sore from the full BiPAP face mask.
One night, spontaneously, my mom wasn’t responsive. My dad was doing the typical inside-the-mouth-wipe-out after her puréed dinner (she had been losing the ability to swallow for two months prior) and I heard my dad yell “Ow!”.
Mom had started rhythmically biting him with a distant gaze ahead and her jaw twitched up and down like a nutcracker.
In the emergency room, we were told she had a spontaneous hypoxic episode, had lost oxygen and her head flooded with carbon dioxide. What they told us next was that she would have to flush out the CO2 with oxygen, and since we had no way to measure her CO2 levels at home, she would need to be monitoring the hospital ICU.
That particular hospital did not have an ICU and they initiated a transfer with our consent to another in-network hospital. What they hadn’t told us was that a patient could be transferred to any hospital or their choosing. In our case, as both family and legal representatives we would have needed to arrange to transport her ourselves.
Had we known this, we would’ve arranged for transportation in Northwestern Medical in downtown Chicago, which is a highly regarded research hospital and happens to be where my mom’s doctors and the ALS clinic are. There, where the hospital staff has training and knowledge of ALS, we would’ve undoubtedly been in better hands.
Unfortunately, this in-network hospital we were sent to was not equipped to safely treat my mom as an ALS patient, and that was apparent when in the first few days we were there and my mom had erratic breathing on the hospital BiPAP, which was prior to the transition to our home BiPAP. I’m thankful that the doctor on staff that week had some knowledge about ALS physiology, but I have no respect for him as a human being, and there’s reasons for that.
Both my dad and I were in the room on that occasion, and another separate time when the nurses adjusted my mom’s BiPAP settings, which exacerbated the problem. The doctor, (who I will refer to as Doctor “X”), came into the room and he told the nursing staff that the settings they had changed should not be used for an ALS patient, and he changed them to what they needed to be.
My dad and I took 12 hour shifts, sometimes overlapping to be with her. We were her voices and both her power of attorneys with dad being the primary and myself being the secondary.
I was horrified at the BiPAP settings incident. Why was it that untrained staff on ALS lung function were allowed to change her settings? This wasn’t our first scare, but it was an event that solidified to me that mom wasn’t safe there. That may sound extreme, but imagine that the doctor hadn’t come in, and due to the incorrect settings causing her respiratory distress, the incident may have potentially caused her death.
One early morning when a single male nurse, who I’ll refer to as, Nurse “B”, had come into our room on his own announced that he would be cleaning up my mom after she had soiled herself, which horrified me.
Only one person on the skeleton, late night, early morning shift was going to do this on their own. It takes three people at home to make sure that she’s safely handled, if she’s being rolled in bed or for any reason. One to hold her upper body, one to support her legs while she’s turned, and one to do the wiping.
I offered to help hold her up that morning. He accepted the help. I had to speak up to request that her head be supported with an additional pillow so her neck wouldn’t be strained. He allowed this as well. But the fact that he hadn’t initiated it was unnerving. I had waited about a minute before speaking up, before she was turned over.
I ended up supporting her legs. In a worst case situation, padding between them might have been sufficient, but as she’s paralyzed, padding won’t keep the upper leg from slipping, which is painful and straining on her body. Nurse “B” pushed her up. While he was wiping her with one hand, mom, who had rarely opened her eyes there due to the hypoxia and the heavy pain meds had her eyes wide open and moaned.
I helped support her upper body with one hand and her upper leg with the other. She’s heavy, and even supporting just her leg requires effort. I stood there both physically and emotionally strained, and my stomach was in knots, and I stood quietly. After that, I placed the wedges behind her back and legs to prop her up on her side while he held her. At that time, she was still using a PureWick in the ICU, which is an external catheter, and the same type we had used at home for years. This one was always on but at home she used to use the eye gaze (Tobii Dynavox AAC) to trigger a button that told our Alexa to turn it on and off.
Nurse “B” had explained to me that she wasn’t urinating very much, so someone would be coming in to do an ultrasound of her bladder and check if, and how much she was retaining urine and if it passed a certain threshold, they would need to drain her bladder with a straight catheter.
Her bladder ended up needing to be drained.
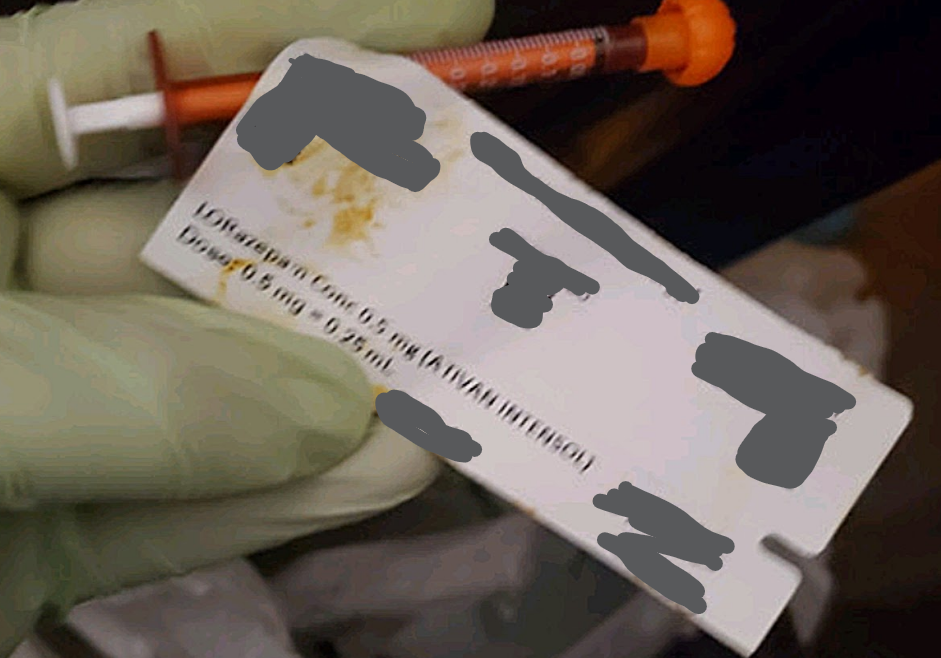
Nurse “B” brought a sterile catheter kit and spread her legs apart. I was sitting on the chair feet from the bed watching. He pulled the PureWick out from between her legs and there was a large stain from the bowel movement he had just cleaned up. He threw the PureWick away, came back to the bed, and started to open the straight catheter container.
I spoke up and asked politely if he would be cleaning her up in front before putting the catheter in. He asked me in a friendly tone if I thought it was just urine on the PureWick. As if he were chuckling or laughing it off. As politely as I could and as awkward as it continued to be I asserted that it looked like a stain from her bowel movement to me. He went to get a couple washcloths.
As he was wiping her with the first washcloth, bowel movement stains continued to dirty the washcloth and he was quiet. His expression turned solemn as he moved onto the second washcloth, and he continued to wipe with more stains gathering.
ALS has been responsible for these throat spasms for years, and one of her ALS clinic doctors had prescribed two medications to combat the muscle spasms. She’s been on them for years since they started. One is Baclofen, which she takes on a daily basis, and the other is liquid Lorazepam. It’s Ativan.
We don’t refer to it as Ativan at home and didn’t even realize for years that it’s the same drug. Our prescription bottles say Lorazepam, and at home we refer to them as “drops” more times than not since it’s a quick way to yell across the house if mom is having a throat spasm. She needs a very small dose, which we set up ahead of time in very thin, small syringes from the bottle to stop the spasm in its tracks.
It only takes a few seconds for the spasms to resolve themselves. I did read early on when she was first prescribed them for treating the muscle spasms, that the medication was a benzodiazepine, which is a strong anxiety medication in the family of drugs that include Xanax and Klonopin, and we keep them on hand with a syringe next to her bed at all times.
When spasms spontaneously happened at home she would gasp for breath, which was a terrifying experience no matter how many times I’d gone through it. We had to fight with the hospital about having them on hand because they told us they couldn’t have “narcotics” open on the floor.
They are controlled substances, like amphetamine ADHD medications. That was what the staff kept repeating though, “narcotics”, and that it violated their regulations to have them on hand on the floor unless they were a scheduled dose that the pharmacy could send up every so many hours. She had never been and still is not currently on a scheduled dose. This is an as needed drug.
Previous to the morning with Nurse “B” and the catheter event, my dad and I had repeatedly reinforced to the staff that when she was having these spasms, she needed the drops ASAP. Between that and the long call bell waits on that day, I had taken an Uber home from the hospital to get sleep and I was so angry that I looked up who I should be reporting this to which I read was the Illinois Department of Public Health.
They have a phone line for complaints, and when I called, it was closed.
I ended up calling an alternate state crisis number, and the woman I spoke to told me that I’d have to call back the IDPH when they opened the next day. I told her on the phone call everything that had been happening. She was empathetic and said in a prior personal experience she had with a parent years ago in a hospital that her family had asked for the floor manager and suggested that I try that for more immediate assistance.
After those calls, I texted my dad and he told me he had a long conversation with Doctor “X” and Doctor “X” said that he would speak with the staff about having medication on the floor. Dad told me not to worry about it and to get some sleep, so I did.
That morning with Nurse “B”, no drops were on hand.
When the spasm started, Nurse “B” stood in the room without a word, so I had asked if he was going to get her the Lorazepam drops, and he told me that he would have to call down to the pharmacy and it was the same situation all over again.
At that moment I posed the question, how about I clean her up and he call the pharmacy? He agreed and handed me an unopened package of wet wipes then left the room without haste.
When I was finished wiping her, I repeated to her that the nurse was getting them as fast as he could and to hang on just a little longer. Her eyes were wide open and she had a blank stare when they were ever since the hypoxic episode. My dad and I weren’t sure she was ever going to recover from that, and I thank God that she has.
I don’t know if she had been hearing me or understanding, but I squeezed her hand while I stood in front of her and it was a miracle despite this horrific situation that whatever physiological change a hypoxia had caused, the spasm episodes which continued until she got the drops had been milder than they had prior to the ER admittance. Despite the respiratory distress and the obvious struggle, she managed to be able to breathe through them.
She had been on the BiPap around the clock and it’s possible the ventilator was helping her through them. I have no idea, but she couldn’t breathe without the BiPAP anymore and still can’t, so she was on it at all times unless she was finishing scheduled nebulizer treatments and with the respiratory therapist across from me, we would have to take the mask off for a moment each time for me to immediately put the cough assist mask on her and hit the start button.
After the machine cycled, plowing air into her lungs and sucking it out, the respiratory therapist would suction the mucus out of her throat that was pulled up by the cough assist and immediately replace the BiPap mask. It was also taken off briefly when she got drops or switched masks.
The hospital did not have a cough assist machine, nor from what any one of the nurses had told me was anyone trained on how to use one. We were asked the first night to bring ours from home.
Nurse “B” gave my mom the drops when he finally came back to the room and the spasm stopped. She had her bladder drained, and I was emotionally exhausted. Mom closed her eyes again.
I sat shaking with my mind racing and I decided to quickly and quietly grab a glove and dig the syringe out of the trash. I had to move the iodine splattered sheets from the straight catheter waste and I couldn’t find it right away. I had my phone camera already opened and when I managed to locate it, I immediately took a picture and placed it back under the other trash.
I also took a picture of the stained PureWick and even went into the dirty laundry bag to take pictures of the washcloths. Then I tossed the glove, went back where I was sitting, wrote every detail from the entire event, and hid my notes in my bag. I had been peering at the clock as everything unfolded and I had started taking notes the previous day to document everything everything that was happening, as I was getting ready to get this report to the IDPH with hopes that they would come to the hospital and investigate.
At that time, it was too early in the morning to call the IDPH, so I asked one of the staff that had come in if I could speak to the floor manager and leader in the morning, a man I’ll refer to as “Z” who was the nurse manager had come into mom’s room to talk to me.
I opened my phone gallery to show him the pictures of the syringe and the PureWick. He held eye contact with me. He wore a face mask and he nodded. As I spoke, he was calm and professional and told me he understood my concerns, and at the end of my grievances, he said he would be able to talk to the nursing staff, but the nurses in the white coats, which turned out to be the advanced practice nurses, he had no authority over.
“Z” said that he would send the “Patient Advocate” to our room to talk. Later that day, a woman I will refer to as “C” arrived shortly after and she handed me her card. The title was not Patient Advocate, but it was someone that had come to hear her concerns, so I expressed them.
It was on the Wednesday that my mom had woken up enough out of her haze to very poorly use the eye gaze that my dad had brought from home with the mount that he had broken down to get in the car. It’s a free standing, heavy rolling base, steel pole floor mount that hangs on at home over her bed with an extended arm.
He reassembled the whole thing in mom’s hospital room prior to that, hoping that if she were to wake up enough she’d be able to speak for herself. Mom was able to type some letters out and hit some buttons, but her eyesight was clearly affected by everything that had happened to her, and she wasn’t able to communicate clearly.
Her pupils shot the gaze points all over the screen and she tried to navigate the keys on the speech program, but she had a lot of trouble. The staff that come in during the time she was using the eye gaze expressed their awe, having never seen a device which someone could speak through using their eyes and they asked questions about it.
When “C” came in, she introduced herself by name, not title, and said that she had heard I “had some feedback” about the ICU and that their ICU had wonderful reviews. I told her flatly that I was sure that’s true, but that hadn’t been our experience thus far. Again, I pulled out the pictures of the syringe in the PureWick.
Her eyes widened and she replied cautiously that taking pictures in the hospital went against hospital policy. That was the start of the many occasions I was told “you can’t take pictures in the hospital”. “C” took me out into the waiting room outside the ICU, and again, I aired my grievances and concerns. She had a notepad and made notes that I couldn’t read.
Her tone was one of empathy and she assured me that all of my complaints would be escalated. She went on to ask me about when mom got the ALS diagnosis and about what we had been through.
She expressed the sentiment that ours was a wonderful story about our family who had cared for my mom and throughout her ALS diagnosis and our strong family bond, and she leaned over and threw her arm around me sitting next to me at the table for this unexpected hug. In that moment I reciprocated when we turned to mom’s room after our talk, she marveled at mom’s eye gaze.
Before she did, I asked her to keep me informed about my concerns and she assured me that she would and was escalating them. That was another thing I hadn’t heard a word about until the, “before-you-leave-with-security” meeting.
“C” came back to our room later that day, my dad and I were both there, and she had changed her tune.
She said she had spoken to the head nurse and was very sharp about us following the rules which were that we weren’t allowed to engage or interfere with the staff care of my mom. That included assisting with three people handling jobs done by less than three people. “C” talked about our concerns and she had no direct answers to the points we brought up.
I mentioned how I had been standing outside my mom’s room when she was having a test done and I was on my phone and clearly able to hear Doctor “X” talking to the nurses at the nursing station about how to read a lung x-ray, and that he thought that “this patient” had pneumonia. He lowered his voice after, and I thought filling in the blanks, regardless of my correctness, that he had whispered, that she wasn’t going to survive, or a similar phrasing, had the high probability of being the last words he finished his comments with.
“C” had walked around that story too, as if she had a doctorate and avoiding questions. Many of the staff performed the same talent while we were there. At times completely ignoring what I had said, going about what they were doing in the room then speaking to me after, as if I had said nothing at all.
At that point I told the story told to me by a former colleague from once she had worked in an ICU and when she first started at the hospital she was hired at that there had been a name on the wall and a chart and the back nursing office, which indicated to give bare bones care to that patient.
She was told by the other nurses that worked there that the doctor was sure this man was going to die in his condition and the staff was directed to allocate their resources into other patients. She even asked to clarify if that patient had a DNR directive and the man didn’t, so she asked if the patient were to have a heart attack, if they were supposed try to save him.
I’m paraphrasing a bit as I can’t recall the terminology she used and this was several years ago. The answer was yes however, they would have to follow protocol and if that man died, he died. They would go through the motions regardless. The memory of that conversation where I was told that story had been tucked away for a very long time, and it made me uneasy to think about under the circumstances.
“Decisions about the allocation of scarce lifesaving treatments must be based on established triage protocols and made by designated triage committees- not individual clinicians at the bedside.” -National Academies of Sciences, Engineering, and Medicine, 2012
Similarly, the NIH COVID-19 Treatment Guidelines reiterate:
“Clinicians should not make unilateral decisions about limiting care; allocation decisions should be transparent, consistent, and guided by ethical frameworks and institutional policies.”
If these doctors truly made predetermined judgements, they violated the very standards meant to protect patients and ensure fair treatment.
It’s this kind of shadowy, behind-the-scenes decision-making disguised as ethical resource management that shatters the trust families place in the healthcare system when their loved ones are most vulnerable.
After telling that story, “C” paused and said nothing like that would happen at their hospital, to which I shrugged, and the conversation moved on to an unresolved note (in regard to our concerns), and our confirming we understood we weren’t allowed to interfere with any of the staff care, or we wouldn’t be allowed to stay in the hospital with mom.
I repeatedly ranted to my dad during the time we were there that my mom must have been a statistic to Doctor “X”, and likely to the rest of the staff. Doctor “X” had the audacity to say after announcing his diagnosis of him thinking mom had “a little bit of pneumonia”, you know, pneumonia is the last stage of ALS, which is completely false.
Not all ALS patients die of pneumonia. It is common but the leading cause of death is respiratory failure. ALS is a terminal disease without a cure and statistically, the life expectancy of a person with a ALS is two to five years after the onset and diagnosis.
The day after the visits from “C”, two nurses came in to turn my mom in her room and clean her up and I asked the main nurse assigned to us that day, I’ll refer to as Nurse “R” to please put another pillow under her head to support it as when they turned her as the one she had under her head was not going to be enough.
Nurse “R” told me my mom would be fine, and they turned her. Mom’s neck was both twisted and bent over with no strength to hold the weight of herself, risking danger of snapping. It was one of those minority moments when mom had her eyes open and she was crying with tears.
What made it even worse was that she was conscious enough that she turned her eyes to look at me while I stood feet from the bed.
I told the nurse that my mom was clearly in pain and I begged her to fold a pillow behind her head to support it. The nurse ignored me. I spoke up again and I said my mom was in pain and crying, and I asked if I could get a pillow or hold her head up.
Those were her exact words.
I stepped aside and to the place she had pointed, and nothing felt real. I hadn’t touched my mom. I wasn’t standing next to either of the nurses. There was no interfering and no breaking the rules yet I was told to step aside. I pushed past my panic after pausing and walked outside the room and called for help. I said my mom needed her head supported and the nurses needed more help.
The nurses at the nursing station stayed seated initially. A couple of them looked at each other and one came to the room in no hurry. By that time Nurse “R” and the other nurse who had been silent the entire time had begun to put the wedges under my mom and had finished cleaning her up. When my mom was in bed, her eyes closed again, and she continued to moan and I said nothing. Neither did any of the three nurses.
The non-emergency police. I told the operator what had just happened and that my mom was being abused and neglected in the ICU right in front of my eyes. She said that she was sending officers to the hospital and confirmed our room number.
My anxiety was through the roof, and I had just called the police.
I could not believe what was happening.
Quoted from my formal report:
“…I dialed the non-emergency police line at 7:40am
Following an incident with [Nurse “R”] in which my mother’s pain and distress were acknowledged but not appropriately addressed, I felt compelled to take further action to ensure her safety. After repeated attempts to resolve these concerns through hospital channels, I contacted the non-emergency [redacted] Police Department to report abuse and neglect.
Two police officers responded to my call. I explained the incident in detail, emphasizing my mother’s pain, the lack of timely intervention, and my ongoing concerns for her safety. The officers informed me that police do not typically address allegations of abuse or neglect within hospital settings. They suggested that I contact a lawyer.”
Wide open. I don’t remember which of the staff had opened them, but they whipped the curtains and pushed them back as far as they could go. After the police left, I asked if I could close the curtains and I was told I could not because it was a “safety issue”.
“…The entire unit could overhear my conversation with the police and my complaints about my mother’s care.
The officers dismissed the photographic evidence and questioned the plausibility of my account regarding improper catheter insertion. No action was taken by the police.”
It was fucking insane.
Doctor “X” walked over and stood directly in the doorway midway into my conversation with one of the officers with his arms crossed and shifting his weight on his feet. He looked disgusted. He stood directly next to three nurses who had repeatedly barked at me, “You can’t take pictures in the hospital” when I had pulled out my phone. One of them literally held the side of the door and the other two were grouped closely behind her, all three of them peering their heads so they could see and one of them pumping her arm in the air behind another in gesture while she spoke.
The second officer who stood in my room and barely spoke had broken his silence after I talked about the catheter to say, “You’re telling me…” about how Nurse “B” was going to put the catheter in my mom while she was dirty, and I. said. yes.
I thought about it later that the officer who had told me straight off the bat that the police don’t deal with abuse and neglect, and they saw nothing in that moment that was happening,
didn’t even take any time to look at my mom to assess her for signs of abuse.
That doesn’t sit right.
The police obviously weren’t taking the situation seriously and I stood there with a mob of people watching. There were staff that had been standing as far back as the nursing station.
I had been so scared in this brand new way from the moment I realized they weren’t going to help us. I had no support. I couldn’t even believe the police hadn’t insisted our conversation be private.
I told the officer that I understood that all he had was my word and I didn’t have a video of what happened that morning before I called but that I still had proof of the syringe and the PureWick and one of the nurses at the door repeated again that it was against the rules to take pictures in the hospital.
I looked over at them then back to the officer and said that if there are no pictures allowed in the hospital, and no security cameras and there is no one watching what happens behind the closed doors of this ICU, how can anyone prove the safety and fair treatment of any one patient?
The officer’s expression shifted to one of more understanding and he said,
There was a moment of unbearable silence, and I initiated the wrap up of the disaster conversation with the officer to thank him for his time and apologized again that he had been sent out when what I called about wasn’t something that the police handled.
I found out then that if I “wasn’t happy” with the “quality of care” that my mom was receiving that we had the right to transfer her to another hospital and I was relieved. I asked for someone to immediately initiate the transfer to Northwestern and “Z” had come to the room very quickly to start the paperwork while I called Northwestern.
When I was on the phone with the neurology department at the ALS clinic I told them my mom desperately needed to be transferred. I got a go ahead call back from the office that my mom’s pulmonologist said it was a good idea, and things were in motion. But they were slow and the longer the process was taking, the more nervous energy filled my stomach with knots.
Nurses began selectively responding to my questions, addressing only those they chose and ignoring others. This created significant obstacles to effective communication and hindered my ability to advocate for my mother’s needs.”
“During this same period, three nurses entered my mother’s room while we were waiting for news about a potential transfer. They took four minutes to administer lorazepam drops, citing the need to check the dose, despite ongoing issues with timely administration.”
I had asked why they hadn’t checked at the start of their shift for details like dosage changes because with my mom’s condition time was a critical variable and my question was ignored. With over two minutes having passed and in distress over mom’s distress during this throat spasm I know that the hospital isn’t trained for an ALS patient the way Northwestern was.
“In response, a nurse in a white coat raised her voice, accused me of calling her ‘uneducated,’ and argued aggressively, talking over me and not allowing me to clarify my statement.
This confrontation was deeply distressing and left me unable to adequately defend myself due to the stress and hostility.
Dr. [“X”] was subsequently informed by two nurses that I had called a nurse “uneducated.”
He stated that he would believe his nurses over me and warned that I could be asked to leave if I impeded my mother’s care.
I clarified my intent, explained the miscommunication, and expressed frustration at the lack of credibility afforded to me as a caregiver and advocate.
Later that day, the head nurse introduced herself and reiterated the importance of respectful communication. She stated that no one wanted me to be escorted out, but I needed to behave respectfully. The conversation was calm, and we parted ways.”
“On June 26, a respiratory therapist approached me regarding the alarm on our home BiPAP machine, which is a new addition to my mother’s care and with which I had not received any training. I explained that I did not want to risk altering any settings and suggested that the doctor, who had configured the machine, be called to safely silence the alarm during my mother’s breathing treatment. Despite hospital policy explicitly prohibiting staff from handling home equipment… The therapist proceeded to touch the BiPAP machine. I asked her to leave the machine and to call the doctor if necessary.
The alarm went off whenever we had taken the mask off to do the cough assist and suction. This particular respiratory therapist (I’ll refer to as “RT T”) was one of the most outrageously cruel people which I had no choice but to interact with while we were there and every day she was on shift I cringed and hoped that her shift was ending soon and one of the other respiratory therapists would be coming in.
A couple days prior to that when I had been switching off with my dad very late night before he went home to sleep he updated me on how the night had been while I was home sleeping.
“On June 28, 2025, at 8:00 PM, the last documented breathing treatment was administered to my mother. At midnight, my father — who is the primary power of attorney — inquired with a nurse about when the next scheduled breathing treatment would be administered, as these treatments are prescribed every four hours which is critical to her treatment.
The nurse claimed that a handwritten note from a team transition (“stand-up”) stated the family had requested no treatments be administered during sleep. My father immediately denied ever making such a request.
The respiratory therapist, [redacted], supported the nurse’s claim regarding the note but refused to provide any information about its origin, including the timestamp, author, or access to the document.
“June 30, 2025 — Around 3:00 p.m.:
I went to kiss my mother and saw that the nostril fit on her BiPAP strap was cutting into her face, leaving prominent red marks. I pressed the nurse call bell and informed the nurse [redacted], pointing out the red strap marks and requesting a change of BiPAP mask.
Throughout her stay, my mother had periodically been switched to the full face “scuba mask” to relieve her face from strap compression and prevent skin injury.
Upon removing the mask, I observed her lips were chapped and cracking, with a yellow fold across the bottom middle (possibly dead skin and mucus), and a deep cut from dryness near the bottom left corner of her lip.
I requested chapstick (already present in the room) be applied to her lips and handed it to the nurse. I also asked for ointment for the deep cut.
Around 3:05–3:16 p.m.:
Nurse [redacted] entered and was asked by [redacted, I’ll refer to her as “Nurse Q”] to get “the tube of light cream.” [redacted] returned with a white tube with blue lettering but stated she could not see where the cut was.”
“Nurse [“Q”] and another female nurse (curly brown hair, pulled back) spent over 10 minutes adjusting the scuba mask, attempting to fit it properly without a leak. This included compressing my mother’s chin into the mask.”
“At approximately 3:07 p.m., [Nurse “Q”] called respiratory therapist [“RT T”] for assistance.
After a few minutes I suggested, ‘Maybe let’s wait for the respiratory therapist.’ [“Nurse Q”] replied, ‘I already called her.’.”
I knew she had already called her because I watched her do it over her voice pager/radio. I was trying to subtly encourage them to stop what was causing my mom this horrible distress. The scuba mask which covered her eyes, nose and mouth was leaking everywhere, the top leak on her forehead caused the plastic to flap and scratch her skin from the air pressure.
“3:16 p.m.:
[“RT T”] (respiratory therapist) entered, stating she was there to do my mother’s breathing treatment. She indicated that the mask would need to be changed back for the treatment.
After the 20-minute breathing treatment, around 3:36 p.m., [“RT T”] began putting the scuba mask back on my mother.”
This woman knew that the nurses were struggling with the mask and this woman said nothing to them about how we would need to change it when she got there back to the original. This was the same woman that scoffed at me when the BiPAP alarm was going off.
This woman was the poster child for retribution.
“[“RT T”] asked me to help put the mask strap on my mother. I questioned why she could not ask another nurse or staff member for help.”
I wasn’t sure if she was setting me up to be hands-on and “impede my mother’s care” so they had a reason to kick me out. It was the only reason I didn’t rush to help. “[“RT T”], with her hand over the mask, replied,
I took a photo with my phone of my mother’s condition and her dropping oxygen levels. [“RT T”] pointed at me and yelled aggressively, ‘You can’t take pictures in the hospital.’”
“Another nurse in the room then assisted instead. All the while my mother’s oxygen levels dropped while the mask was delayed being put on.”
I had my phone in hand which I had picked up when I moved the tray with the cough assist machine on it away and as this woman had one hand hardly holding the mask on my mom’s face and while she shrugged “Whatever!” I unlocked my phone as fast as I could and took a picture that included the vitals monitor which shows how low my mom’s oxygen had dropped.
I got through, and spoke very quietly and my heart beat so fast that I could feel my chest trembling while I was talking. I didn’t know where to start and I told this person on the phone that I was trying to speak quietly because I didn’t have privacy in the hospital room and he didn’t seem to be hearing what I was trying to say because he was taking what I said as if I had been reporting about a lack of privacy.
I kept stumbling to interject and clarify while he talked over me and he said I could always file a complaint to the complaint department email which he read to me
Then the call ended.
I sat there in that chair for I don’t know how long and by that time everyone else had left the room. Nurse “Q”, who had been assigned to us that day, had come in quietly and I turned to her and thanked her for being so attentive to my mom and genuinely appreciated her help.
I had thanked her throughout the day, and at that time wanted to ease any nervousness she may have had as she was one of the staff in the room that undoubtedly heard me on the phone stating that I wanted to file a complaint against the hospital.
“At 10:30 a.m., I was in my mother’s ICU room and observed her arterial blood pressure was critically low at 73/35. I immediately rang the call bell at 10:31 a.m. for nurse assistance. A staff member came by, said they would get someone to check in with us, and left. At 10:32 a.m., her blood pressure was still low at 93/40, and at 10:33 a.m., it was 96/41.
She also stated that she was ‘doing rounds’ at the time I rang the nurse call bell.
Between 8:40 and 9:00 a.m., there was high activity in the room, but I was not given any clear communication about what medications or interventions were being administered.
At 10:38 a.m. Nurse [redacted, I’ll refer to as “D”], our assigned nurse for the day, entered the room. I raised my concern for my mother’s blood pressure as well as said that two or three days prior, another nurse told me the ICU staff had turned off my mother’s arterial blood pressure alarm because it was going off so frequently. The day before I was told this, I witnessed the alarm going off every few minutes while her blood pressure fluctuated dangerously. When I asked [Nurse “D”] at 10:38 a.m. if the alarm was on, she said it was.
[Nurse “D”] also told me that at 10:20 a.m. she had given my mother a one-time dose of Midodrine, a medication to raise blood pressure.
I was not informed beforehand that this medication was scheduled or administered. As my mother’s legal representative and advocate, I should have been notified, especially since my mother was incapacitated and unable to communicate.
[Nurse “D”] said the Midodrine had been scheduled sometime between the previous night and that morning, but could not specify exactly when, and that it had been given at 8:30 a.m. via her g-tube. I was not aware of any of this prior to our conversation.
Earlier in the morning, at 6:54 a.m., [Another nurse, redacted] told me Tylenol would be given at 9:00 a.m. There was no mention of Midodrine or any other medication.”
“At 11:00 a.m., respiratory therapist [redacted, not the one from the previous incidents, and one I couldn’t have appreciated more] and Nurse [“D”] came in; my mother’s blood pressure was 148/67. They said they were going to transition my mother from the hospital BiPAP to our home BiPAP machine. I asked if either of them was trained on our home BiPAP, and both said no. I requested that the doctor, who had previously made changes to her settings, come and perform the transition.
Around 11:05 a.m., Doctor [redacted, I’ll refer to him as Doctor “V”] entered and began setting up the BiPAP without speaking to me until after the procedure. I was on the phone with my father, trying to explain the situation, which led to some confusion and a brief argument on speakerphone. After the transition, I apologized to Doctor [“V”] for the confusion; he acknowledged the difficulty and left.”
This was a new doctor working in the ICU than the previous week. He was generally quiet, not friendly but hadn’t yet become unfriendly either.
“At 11:21 a.m., I asked Doctor [“V”] for a copy of the incident report from the prior Thursday night hypoxic episode (caused by a staff member closing the BiPAP ventilation cap). My father was present, I was not). He told me I could not access that report or any medical records until my mother was discharged.
At 11:25 a.m., my mother’s arterial blood pressure was 200 (systolic), and she was moaning and visibly distressed. I took a video of her fluctuating blood pressure. At 11:26 a.m., I pressed the call bell again for nurse assistance as her blood pressure reached 202/201, and she was still in distress. No alarm sounded on the monitor despite these readings. The doctor and respiratory team had left after the BiPAP transition, and no staff remained in the room to monitor my mother.
Nurse [redacted] (unsure of full name, but the first letter on her badge was “[redacted]”) entered after my call bell. I expressed my concern about the high arterial blood pressure. Nurse [redacted] told me the arterial number could not be correct and that the ICU staff were relying on the cuff blood pressure, not the arterial, because the arterial readings fluctuated so much. She said she would get someone to come in, but before leaving, she was focused on the monitor. No one came to check on my mother’s blood pressure cuff or her status until Advanced Practice Nurse [redacted, I’ll refer to as “APN G”] arrived at 11:35 a.m. — nine minutes after my call bell activation for a hypertensive crisis.
Nurse [“APN G”] entered my mother’s ICU room. She confirmed that the staff were aware my mother’s blood pressure was high and explained that they could see her monitor readings from the nursing station. [“APN G”] stated that the staff were not relying on her arterial blood pressure readings, but instead were monitoring her cuff blood pressure measurements.
[“APN G”] explained that my mother’s positioning could affect the accuracy of her arterial blood pressure readings. I referenced an event from June 30th, when our nurse [“Q”] had repositioned my mother onto her back in the afternoon to reset the arterial blood pressure line, and at that time, the arterial and cuff readings had somewhat matched. [“APN G”] agreed, stating that when you reset the arterial line, the numbers usually align.
I asked if the staff were going to reset my mother’s arterial blood pressure line at that time. [“APN G”] did not respond to this question. I then asked if she or another staff member would run a cuff blood pressure measurement, but again, she did not answer. Instead, she explained that Midodrine increases blood pressure and that it had been given to my mother because her blood pressure had been very low.
I acknowledged that I had been told about the Midodrine after the fact, but expressed my concern that no one had informed me about either dose, or even that the medication was being given at all. I specifically asked who wrote the order for Midodrine, but was not told, despite my inquiry.
[“APN G”] attempted to reassure me that the staff were monitoring the cuff blood pressure readings.
I voiced my concern that it was alarming no one would check the cuff blood pressure if the alarm went off, and mentioned that a few days earlier, a nurse had told me the arterial blood pressure alarm had been turned off due to frequent fluctuations.
I emphasized my concerns about the situation and expressed that I wanted to be on the same page as the staff and treatment protocol. [“APN G”] responded with understanding and an upbeat demeanor. I asked for confirmation that the staff were actively monitoring my mother and were not concerned with the arterial blood pressure readings. [“APN G”] confirmed both, and our conversation concluded at 11:37 a.m.”
“(Context background 8:25 a.m.:)
I asked Nurse [“D”] if [“Z”], the nurse manager, was working that day. [Nurse “D”] confirmed she had seen him and informed him that I wished to speak with him regarding an incident from June 30th (unrelated to July 1st events).”
“[”Z”] entered my mother’s room while I was present alone with her. He asked, “What’s going on?” and I explained the June 30th incident, as well as my ongoing concerns and the conflicting information I had received on July 1st.
While discussing these concerns, I noticed a leak in my mother’s BiPAP mask; her lip was hanging out of the mask. I rang the nurse call bell. Doctor [“V”] entered the room. I informed him about the mask leak and my mother’s lip position.
I requested that Doctor [“V”] wear gloves, as I did not know if he had washed his hands, but I had not seen this. He eventually put on gloves, and together with [“Z”], adjusted the mask fit.”
The doctor seemed to snap when I asked him to wear gloves. He expressed his offense that I would “say” he didn’t as well as stated that he had. I replied that I hadn’t seen him and thanked him for putting on gloves regardless. You’d have thought I’d slapped him the way he shot back at me.
“I raised my concerns about my mother’s blood pressure and the administration of Midodrine, for which I had not been given information or consented to Doctor [“V”]. He stated that my mothers blood pressure had been very low and she had received two doses of Midodrine close together, which would explain her high blood pressure, and stated it’s not right to give her more medication to offset her high blood pressure, which I agreed, and noted I was not asking for medication and was requesting her blood pressure cuff be run and she be assessed.
I suggested that my mother’s blood pressure could also be elevated due to pain.
I was astonished by the question with his demeanor.”
I absolutely could not believe that he could have said that, and my tone flattened. I asked him to confirm for clarity that he nor anyone else was going to do anything for her extremely high blood pressure.
“Doctor [“V”] confirmed he would do nothing for her blood pressure.
I clarified that I had never asked for anyone else/in particular.
After the doctor left, I stepped outside the door of the room where [“Z”], [“C”], Doctor [“V”] and a couple other staff were present in the nursing station area. I asked [“Z”] if he would provide a written statement reiterating the doctor’s comment about staff being too busy for me to ring the call bell. [“Z”], along with [“C”] (the patient advocate, who was not present in the room during the comment), and Doctor [“V”], all verbally denied that such a statement had been made while raising their voices.”
The night before I had sacrificed a considerable amount of sleep going back through all of my documentation and familiarizing myself with every state and federal regulation that applied to our situation, in particular, patient rights.
“Doctor [“V”] then approached me aggressively, standing uncomfortably close, and accused me of putting words in his mouth. He stated he was offended and denied making the statements I described. I responded that his aggressive, confrontational behavior violated my mother’s and my patient rights. He insisted it did not and walked away.
I stated I would look up the law on my phone to read it to him;
I told him he was welcome to do so and began to look up patient rights on my phone.
and an officer who was already present at the nurses’ desk approached my room.
I called my father, explained the situation, and decided to leave on my own accord. My father agreed and said he would come to the hospital early to take my place. I collected my belongings, announced to the ICU staff that I was leaving voluntarily, and asked the security guard if he was ready to walk me out.”
My dad was calm and told me to make sure I took all our electronics with me and said mom would be fine, not to worry, and he would get ready to head over. I kissed my mom and I told her that my dad would be there soon and I would see her soon too. She was asleep or seemed to be, but if she was listening, I wanted to comfort her so she wouldn’t be scared.
As I stepped out of the room I announced I was leaving on my own accord. Then,
I was lugging 3 heavy bags through the hallway with me when “C” asked to talk before I left and I didn’t turn to look at her when I replied. I kept moving. I glanced at her when she asked if I’d like help carrying one of them and I declined. There was a massive amount of tension in the air. I had no idea what to expect, but both “C” and “Z” didn’t seem to have a threatening air about them at the time and “Z” asked if I wanted something to drink when we entered the room.
“C” and I sat down and “Z” returned with three waters that sat in plastic cups with lids and straws he left the paper tips on as well as two small soda cans which sat untouched as we spoke.
“[“C”] acknowledged that my claims were serious — abuse, neglect, and malpractice — and wanted to listen. She took out a notebook. I discussed my concerns about monitoring and alarm management as well as the 6/30 incident with [“RT T”]. [“C”] asked if I had discussed the blood pressure issue with the doctor and how I knew my mother’s blood pressure was high.”
“[“Z”] explained the clinical rationale for the administration and dosage of Midodrine. [“C”] questioned why I had not brought these concerns to her earlier. I explained that after reporting [“Nurse B”’s] behavior earlier (improper cleaning, HIPPA violation — see previous report), he was back at work the next day, despite assurances that my concerns would be investigated and escalated, which undermined my trust in the process.
I showed a photo of my mother’s dry, red, and chapped lips and red marks from the mask straps from prolonged BiPAP use without proper care, and
The conversation continued, and I eventually asked [“C”] if she would provide her written consent for me to record the rest of the conversation.
I responded that I would continue the conversation after consulting legal advice.”
I stood up, picked up my bags, opened the door, said nothing more to “Z” or “C”, who stayed seated without another word and with a nod, I started to walk alongside the very, very tall security guard toward the elevators who spoke only twice during the walk.
First was at the elevators.
I headed toward the ones I used when I would leave and come back, and the guard directed me to a separate set of elevators on the opposite side. What threw me for a loop was that after I stepped into the elevator, I turned around to wait for the guard who had opened the door to the stairs across from the elevator door while gesturing his intention by pointing at the open door.
He looked like he was quietly talking into his radio or about to. The elevator door closed after the stairway door had, and I made it to the lobby floor before he did.
So for a moment, I stood there waiting for him. It was a short walk to the hospital entrance and I told him I needed to call an Uber home. Instead of waiting with me, he walked me to the sliding doors at the entryway and gestured outside while telling me there was a bench that I could sit on and set up my Uber.
“I called my father to inform him I was leaving the ICU. At the time of my departure, and leading up to it, there were no nurses present in my mother’s room. According to the medication records later reviewed and told to me by Nurse [“D”] upon my request to know when the last time it was given, my mother was administered Narco-as-needed pain medication at 2:00 p.m., (July 1st) after I had left the hospital.
My dad was still home getting ready to go when I got home and after a short talk I collapsed into my bed and felt a mixture of nervous energy and exhaustion.
I sent an email from my computer to “Z” gently asking him if he had time before his shifts end if he had time if he wouldn’t mind stopping by my mom’s room in case any of the nurses needed help with my mom’s mask,
which reads,
“The patient or his or her representative (as allowed under State law) has the right to make informed decisions regarding his or her care. The patient’s rights include being informed of his or her health status, being involved in care planning and treatment, and being able to request or refuse treatment. This right must not be construed as a mechanism to demand the provision of treatment or services deemed medically unnecessary or inappropriate.”
My dad answers his phone on speaker more than half of the time, so when he picked up an unexpected incoming call and I heard “C”’s voice I was suddenly alert. I could only make out a few words of hers, and some of my dads who had been talking two rooms away, but the tone of the conversation sounded both awkward and friendly.
I overheard bits of my dad saying that he heard what happened at the hospital and that he would be heading over shortly. They spoke for several minutes. When their call was over my dad walked to my room and I asked him what was said.
His recap included that she told him when I left the hospital I was very upset, to which my dad casually told her that I was emotional about my mom’s condition and she wanted to know if she could speak with me and apologize to which my dad had told her just as casually that I was in bed and it was best to let me cool down.
I was curious what wording she used and what story she had told him and what details she disclosed or withheld, but being exhausted, when he said after he thought everything would be fine, that he was heading out, and that he would ask while he was at the hospital if I would be able to come back, I let sleep take me.
I woke up late at night when I typically had been to get ready to go and switch places with him and nervously asked if there was any word. He said I would be able to come in after the morning shift change. That was welcome news, and in the morning my Uber dropped me off a few minutes early, so I deliberately sat in the lobby until the exact minute in which was agreed upon for my return.
I texted my dad I was downstairs and he had told me he had gone to the nursing station desk to remind the secretary I would be coming up, who he said “made a face”. He said he made sure she too had a copy of the Power of Attorney paperwork and reminded her I was on it. He stayed for some time after I had gotten there to make sure there were no issues and napped in the visitors’ recliner parallel to my mom’s bed, and I thought to myself as I often had how sweet it is how much he loves my mom.
“July 2, 2025, 9:49 a.m.:
I inquired with staff about the last administration of Narco to my mother. [redacted], a staff member, checked the records and informed me that the last dose was given at 2:00 p.m. on July 1. I had not been informed of this administration at the time, nor was I consulted or asked for consent in my capacity as my mother’s legal guardian and secondary power of attorney.”
There had been more that had happened than what I’ve written here and nonetheless I had documented.
I read to her, I held her hand, I talked to her endlessly, everything I could remember she had told me long ago that people had done with their loved ones who were in comas that had woken up from them.
I streamed movies I knew she liked on my iPad.
Even with her eyes closed I positioned the iPad on a rolling tray best I could. If she were to open her eyes, she’d be able to see the screen.
I even put my head next to hers and tested the volume so I could see if she could hear from the distance.
I was not ready to lose my mom, not that I ever will be, and I knew that I could, and can. I had thought that I was moments away from losing her in the hospital a thousand times.
I played Reiki videos in her room on YouTube and prayed and prayed and prayed.
I prayed a shitton.
I told God he could take me in her place if he would please let her live and I prayed for her to recover and I prayed more than anything to help her be able to come home so if she had to die she could do it at home with our family in her bed and we could all be together. Even if it was just for a day.
I prayed to God, Jesus, the Virgin Mary, St. Joseph, St. Jude, St. Anthony, Padre Pio, St. Joan of Arc, St. Dymphna, St. Peter, St. Expedite, St. Alice, St. Lucy, St. Gerard, St. Hernandez, Archangel Gabriel, Archangel Raphael, Archangel Michael, St. Benedict, St. Bernadette, St. Peregrine, St. Christopher, St. Francis and asked my grandparents who had passed to please help my mom and heal her and I am eternally thankful to each and every one of them, and pray daily for help and thank them for everything they’ve done and do for us. They’re all very kind saints which I recommend sending a prayer up to if you’re in need of help.
I mean, if you don’t buy a ticket, you have no chance of winning. If you buy a ticket, you spend maybe a few dollars with no guarantees you’ll win, but you’ve spent a couple dollars out of your wallet for a chance. Instead of dollars, I spend a couple minutes praying, and I invest in a chance for a little higher up help.
It was the best analogy I could think of at the time, and I think it still holds up pretty well.
Anyway, we took mom home on hospice from the hospital, and she’s recovered tenfold from the state she was in while there. The antibiotics she was given had worked to clear up the pneumonia.
There are still a whole lot of frightening moments for all four of us at home, and many challenges both new and old, but my mom at the time in which I am writing this article is alive, in our living room in her hospital bed and sleeping on her BiPAP which she still relies on to breathe.
I love my mom.
My mom’s will to live is and has been so incredibly strong, and I tell her every day how strong and wonderful of a mom she is and how I’m so proud of her and how much I love her, and every time she tells me on her eye gaze (which she can use now just as she could before the ICU) that she loves me too,
I am so filled with joy and gratitude because I did not think I would ever hear her tell me she loved me again at the end of June.
Mom beat the odds, and I am forever grateful she pulled through and came home safe. Nothing has been ordinary for the past four and a half years, and with luck, maybe a little help from above and maybe just the universe looking out for us, I hope to have much more time with her still.